Death is not a fixed moment in time. Brain cells can take many hours to die. It is a misconception even among doctors that the body dies all at once. We are only a little dead when even an hour after the heart has stopped.
Raising the dead may soon become medical reality. According to critical care physician Sam Parnia, modern resuscitation science will soon allow doctors to reanimate people up to 24 hours after their death.
In the past decade we have seen tremendous progress. With today’s medicine, we can bring people back to life up to one, maybe two hours, sometimes even longer, after their heart stopped beating and they have thus died by circulatory failure. In the future, we will likely get better at reversing death. We may have injectable drugs that slow the process of cell death in the brain and other organs. It is possible that in 20 years, we may be able to restore people to life 12 hours or maybe even 24 hours after they have died. You could call that resurrection, if you will. But I still call it resuscitation science.
There is no generally enforced standard of care. In some communities in the United States, survival rates after resuscitation are as low as close to 0 percent. In general, we are better at rescuing people who suffer cardiac arrest in hospitals. But even in this group the average now in the US is 18 percent. The United Kingdom has 16 percent and I assume German hospitals have a similar rate.
Parnia: Here in Stony Brook we had a 21 percent survival rate when I first arrived. Now, two years later, we are at 33 percent. In the first quarter of this year, our latest available data shows that we reached 38 percent, which likely puts us among the top hospitals in the US. Most, but not all of our patients, get discharged with no neurological damage whatsoever.
A recent study found that the optimal length of resuscitation to yield higher survival is at least 40 minutes. Yet most doctors will stop within 20 minutes. They don’t try as hard because they wrongly think the brain will be damaged by then or that it will be pointless to continue.
Resuscitation has gone from something every doctor does every now and then to a highly specialized and complicated field, much like cardiology. Yet that is not generally recognized. As long as hospitals don’t require their resuscitation doctors to implement all the nuances required to save brains and lives after cardiac arrest through fully trained specialists, survival rates in general will not improve. I think we need more regulation by state or medical authorities. That’s the only way to reach higher standards. We can’t go on with a situation where hospital or individual physicians decide for themselves what part of the guidelines they implement or not.
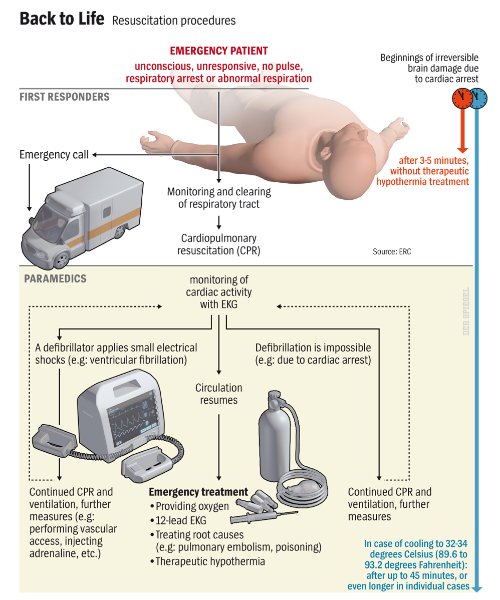
SPIEGEL: Basic first aid teaches us that the brain is very fragile. Three to five minutes after the heart stops, the brain incurs permanent damage due to lack of oxygen.
Parnia: This is a widely-held misconception, even among doctors. It’s mostly based on research done in the 1940s, 1950s and 1960s. In those days, doctors concluded that brain cell death was inevitable in such a short time. Now we know that if treatment is correct, it really can take hours for brain cells to die. And only if all the treatments that we know today are not implemented, the damage can become apparent after as little as five minutes without blood flow. Part of the problem is that we all live in the past — patients, doctors, nurses and legislatures. We have preconceived ideas about death. For thousands of years, death was a clear, precise moment: The heart stopped beating, and that was it. Nothing could be done from then on. You either were alive or not. But since the arrival of CPR (cardiopulmonary resuscitation) more than 50 years ago, we know that this view is no longer correct. Death is not a fixed moment anymore. From a cellular perspective, it is a process that proceeds at various speeds in the different tissues of the body after the heart stops.
It is of paramount importance to protect the brain. CPR as early as possible after cardiac arrest is essential. But the really dangerous period for brain is only after you restart the heart and get the person back to life. It is then that you start getting major brain damage. One of the reasons for this is that when you restart blood flow to the brain, which hasn’t seen any blood for a while, the oxygen itself becomes toxic. The brain can become very swollen and inflamed and at the same time, blood flow to the brain drops to dangerously low levels. The brain also becomes perilously starved of oxygen and nutrients. Consequently, most brain damage after resuscitation occurs not within the first few minutes of death, but in the hours up to the first 72 hours after resuscitation. But with proper post resuscitation care, we can minimize that.
SPIEGEL: What can you do to potentially bring him back to life?
Parnia: It is a chain of interventions, and everything we do counts. One error somewhere along the line, and he will stay dead or live with brain damage. We start with chest compressions as early as possible, first by hand, then by a machine, because in general human beings cannot administer this to the required standards for more that just a few minutes. At the same time we provide breaths via an ambu bag — not more than 8 breaths per minute. Even this simple exercise is often done wrong in many cases. Once you pump too much air into the body, it squeezes the heart, and it won’t start again. This itself can kill people — or in this case, keep them dead.
SPIEGEL: What are some of the newer interventions that you’d recommend?
Parnia: We cool the body down, from 37 degrees to somewhere between 32 and 34 degrees. I usually go to 32 degrees. Patients stay at this temperature for 24 hours or so. Cooling has a lot of positive effects. It reduces the amount of oxygen the brain needs, it prevents dangerous chemicals like hydrogen peroxyde from forming and it slows down the process of cell death. Even this really critical part of resuscitation is not done routinely, not even in places where its benefits are known, including Germany. At times it has been reported to be used by less than 50-60 percent of hospitals.
SPIEGEL: How do you cool a body?
Parnia: We use pads that get attached to the thighs and the upper body. In a matter of hours, the cooling machine brings the body temperature down to the desired level. But you could also do this at home, if you found someone there in cardiac arrest. Call an ambulance, administer CPR and place a bag of frozen peas or other frozen vegetables on the patient. It helps to protect the brain.
The reality is that preserving the brain requires brain experts with specialization in this field, as it is very complicated. Saving lives also requires experts in ventilator management, together with cardiac experts. No physician can be expected to be a specialist in three different areas of medicine so each does the best they can from their own perspective. With such a complicated condition the solution is to have national and professional responsible bodies to enforce and train specialists to deal with resuscitation based on 21st century standards and not 20th century ones. Rightly used, reanimation could play a major role in the therapy for many life threatening conditions and thousands more will be saved.
In my view, young, otherwise healthy people shouldn’t die from heart attacks anymore. Remember James Gandolfini, the actor from “The Sopranos” who died last month at age 51 in Rome? I believe if he died here, he could still be alive. We’d cool him down, put him on ECMO, so oxygen gets to the tissues and prevents them from dying. Clinically dead, he could then be cared for by the cardiologist. He would make an angiogram, find the clot, take it out, put in a stent and we would restart the heart.
SPIEGEL: Is this truly a realistic scenario?
Parnia: Of course we can’t rescue everybody, and many people with heart attacks have other major problems. But I will say that if all the latest medical technologies and training had been implemented, which clearly hasn’t been done, then in principle the only people who should die and stay dead are those that have an underlying condition that is untreatable. A heart attack is treatable. Blood loss as well. A terminal cancer isn’t, neither are many infections with multiresistant pathogens. In these cases, even if we’d restart the heart, it would stop again and again.
If you liked this article, please give it a quick review on ycombinator or StumbleUpon. Thanks

Brian Wang is a Futurist Thought Leader and a popular Science blogger with 1 million readers per month. His blog Nextbigfuture.com is ranked #1 Science News Blog. It covers many disruptive technology and trends including Space, Robotics, Artificial Intelligence, Medicine, Anti-aging Biotechnology, and Nanotechnology.
Known for identifying cutting edge technologies, he is currently a Co-Founder of a startup and fundraiser for high potential early-stage companies. He is the Head of Research for Allocations for deep technology investments and an Angel Investor at Space Angels.
A frequent speaker at corporations, he has been a TEDx speaker, a Singularity University speaker and guest at numerous interviews for radio and podcasts. He is open to public speaking and advising engagements.